
"I couldn't get out of bed." Worse, "I had a newborn I was unable to care for," she says. "I had a fever, cramping and fatigue," she says. diff, which lingered for six months, through three recurrences. Shortly after giving birth to a baby girl, Warren, 39, developed the epidemic strain of C. Instead of isolating the roommate, the hospital allowed her to stay with Warren, even sharing a bathroom, where Warren probably contracted the disease. diff than food products.When Amy Warren of Maineville, Ohio, was hospitalized for preterm labor treatment in 2004, she had a roommate who exhibited C. Lax hand hygiene, improperly cleaned hospital rooms and overuse of antibiotics are far more likely to transmit C. diff infection should pay closest attention to hospitals and health care settings, Gerding said.
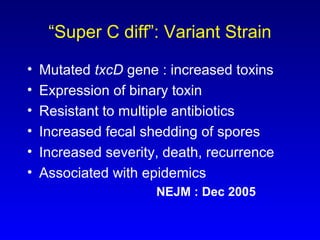
"After seeing her with the bad cramping, I don't want to see her like that again." "I'll cut back, probably, on my meat eating," she said. diff has been detected in meat made Woodard think twice, despite CDC assurances to the contrary. Woodard is scared the infection will return, or that it will strike one of her other grandchildren. But she wound up doubled over on the floor with severe cramps and diarrhea for nearly two weeks, until a clinic cultured her stool and diagnosed the illness. The child hadn't had antibiotics for six months and she'd been nowhere near a hospital or health center. That's little comfort to Mary Woodard, 51, of Rock Falls, Ill., whose 6-year-old granddaughter, Nichole Lilly, contracted a C. diff can't be traced quickly to its source. coli 0157:H7, which has transmitted illness through foods from ground beef to fresh spinach, C. diff is a tricky bug, hard to kill with anything but bleach in the hospital and able to survive most cooking techniques in the kitchen. “It may well be that retail meats are a source or the main source.”Ĭ. “For these community-associated sources, there has to be a source outside the hospitals,” Songer said. Recent victims have included a 10-year-old girl with no history of antibiotic use who became very ill but recovered and a 31-year-old woman pregnant with twins who spontaneously aborted her babies and then died after becoming infected, according to a 2005 review by the CDC. It’s not clear, however, where the remaining infections - those that occur outside health settings, in the community - originate. diff infection can destroy the colon and lead to blood poisoning and death. It can cause severe, repeated diarrhea that resists all but the most powerful drugs. About 13 in every 1,000 hospital patients is infected or colonized with the bacteria, a rate between 6.5 and 20 times higher than previously estimated, according to figures released last week by the Association for Professionals in Infection Control and Epidemiology, or APIC.Įvery day, those infections likely cost $32 million, on average, and claim more than 300 lives, the study showed.Įspecially worrisome has been a new, more virulent strain, called NAP1, which produces about 20 times the toxins of ordinary strains.

difficile infections now occur in hospital or health care settings - and the number of infections is rising. But overuse of antibiotics has allowed the germ to develop resistance in recent years, doctors said, creating the toxic new type that stumps traditional treatment.Ībout 80 percent of C.
About 3 percent of healthy adults harbor the bacteria with no problem. diff has long been a common, usually benign bug associated with simple, easily treated diarrhea in older patients in hospitals and nursing homes. diff spores were toxinotype V, a type linked to illness in pigs and calves and, increasingly, in humans, Songer noted.Ĩ0 percent of infections occur in hospitalsĬ. Contamination ranged from 41 percent of pork products and 44 percent of turkey products to 50 percent of ground beef samples and more than 62 percent of samples of braunschweiger, a type of liverwurst. Songer's samples included brands sold in grocery stores across the nation. difficile has been found in some retail meats, that possibility does exist.” Clifford McDonald, chief of prevention and response for a division of the CDC. “There are no documented cases of people getting Clostridium difficile infection from eating food that contains C. diff bacteria and infection has not been established and that there’s not enough evidence about food transmission to warrant public alarm. diff said the connection between the presence of C. Glenn Songer, a professor of veterinary science at the Tucson school, who talked with about work now under review by the federal Centers for Disease Control and Prevention.īut specialists from the CDC and scientists who study C. “These data suggest that domestic animals, by way of retail meats, may be a source of C.


 0 kommentar(er)
0 kommentar(er)
